Baxter Presents Data Indicating Sharesource Increases Patients’ Time on Home Dialysis by More Than Three Months
Increased time on therapy is an important indicator that remote patient management can improve clinical effectiveness and quality of care for kidney patients on home dialysis
The new data is part of a growing body of evidence that Sharesource can support enhanced home dialysis care
Deerfield -
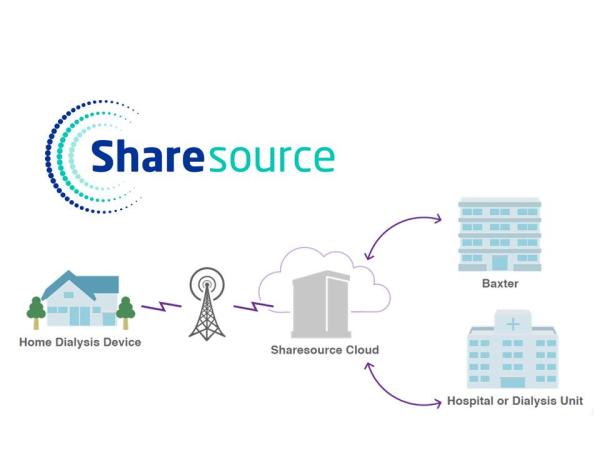
Baxter International Inc. (NYSE:BAX), a global innovator in kidney care, announced today new data indicating the use of Baxter’s Sharesource remote patient management platform with an automated peritoneal dialysis (APD) cycler may improve the clinical effectiveness of home kidney patients care by extending their time on therapy by 3.4 months.
The new data was presented during the World Congress of Nephrology, February 24-27, in abstract session, “Time on Therapy in Automated Peritoneal Dialysis Patients with and without Remote Patient Monitoring Program: A Propensity Score Matching Cohort Study,” [WCN22-0340].1 The retrospective study included nearly 1,500 home peritoneal dialysis (PD) patients receiving care at Baxter Renal Care Services clinics in Colombia and took place between 2017 and 2019, with a two-year follow up in 2021.
“Time on therapy is one of the most important indicators of clinical effectiveness and quality improvement for home kidney patients using remote patient management,” said Peter Rutherford, MB BS, PhD., vice president, Medical Affairs, Baxter Renal Care. “Sharesource is a valuable tool in enabling healthcare professionals’ visibility and timely support of their home patients, which is a key factor in a growing body of clinical evidence that the digital health platform is supporting enhanced care.”
Sharesource, which allows healthcare professionals to monitor their patients’ home dialysis treatments, and then remotely adjust therapy without the need for patients to make unplanned visits to the clinic, has also been shown to reduce hospitalizations and costs, travel to clinical facilities and wait times. 2,3,4,5,6
The time on therapy study presented at the World Congress of Nephrology was a retrospective cohort study of incident patients (defined as those who reached and continued APD from day 90), comparing outcomes for those receiving APD with or without remote patient management. The methodology included time until death, with censorship for technique failure, kidney transplantation, treatment suspension, abandoned therapy or transferred to a different clinic. Using the propensity score matching procedure, an adequate balance in the predictive variables was achieved. The results indicate a statistically significant difference in the time on therapy, which was 18.9 months in the group on remote patient management versus 15.5 months in the group without. There was no statistically significant difference in the mortality rate.
Sharesource is available on Baxter’s Homechoice Claria and Amia APD systems in Canada and the United States; with Homechoice Claria APD systems across select Asia Pacific, European, and Latin American countries; and the Kaguya APD system in Japan. In total, Sharesource is currently serving more than 50,000 patients, across more than 70 countries.
About Peritoneal Dialysis
People living with end-stage renal disease require dialysis treatment or a kidney transplant to stay alive. PD therapy is typically managed by patients in their home, at a time of day that is convenient for them. It works by cleaning the blood of toxins and removing extra fluid through the body’s peritoneal cavity. Studies show patients and physicians often prefer home dialysis.7 PD patients experience improved early survival, and higher satisfaction rates and quality-of-life measures.8,9,10
About Baxter
Every day, millions of patients, caregivers and healthcare providers rely on Baxter’s leading portfolio of diagnostic, critical care, kidney care, nutrition, hospital and surgical products used across patient homes, hospitals, physician offices and other sites of care. For 90 years, we’ve been operating at the critical intersection where innovations that save and sustain lives meet the healthcare providers who make it happen. With products, digital health solutions and therapies available in more than 100 countries, Baxter’s employees worldwide are now building upon the company’s rich heritage of medical breakthroughs to advance the next generation of transformative healthcare innovations. To learn more, visit www.baxter.com and follow us on Twitter, LinkedIn and Facebook.
This release includes forward-looking statements concerning potential benefits associated with Sharesource, Amia, Homechoice Claria or Kaguya. The statements are based on assumptions about many important factors, including the following, which could cause actual results to differ materially from those in the forward-looking statements: demand for and market acceptance for new and existing products; product development risks; inability to create additional production capacity in a timely manner or the occurrence of other manufacturing or supply difficulties (including as a result of natural disasters, public health crises and epidemics/pandemics, regulatory actions or otherwise); satisfaction of regulatory and other requirements; actions of regulatory bodies and other governmental authorities; product quality, manufacturing or supply, or patient safety issues; changes in law and regulations; and other risks identified in Baxter's most recent filing on Form 10-K and Form 10-Q and other SEC filings, all of which are available on Baxter's website. Baxter does not undertake to update its forward-looking statements.
Baxter, Sharesource, Amia, Homechoice Claria and Kaguya are registered trademarks of Baxter International Inc.
1 Sanabria M, et al. Time on Therapy in Automated Peritoneal Dialysis Patients with and without Remote Patient Monitoring Program: A Propensity Score Matching Cohort Study. Abstract presented at World Nephrology Congress. Virtual. 2022. [WCN22-0340].
2 Darkins, A, et al. Care Coordination/Home Telehealth: The systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemed. J. E. Health. 14, 1118–26 (2008).
3 Broderick, A, and Lindeman, D. Scaling Telehealth Programs: Lessons from Early Adopters. The Commonwealth Fund. 1–10 (2013). Case Study.
4 Clarke, M, Shah, A, Sharma, U. Systematic review of studies on telemonitoring of patients with congestive heart failure: A meta-analysis. J. Telemed. Telecare 17, 7–14 (2011).
5 Inglis, SC, Clark, RA, McAlister, FA, Stewart, S, Cleland, JGF. Which components of heart failure programmes are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients: Abridged Coc. Eur. J. Heart Fail. 13, 1028–40 (2011).
6 Klersy, C, De Silvestri, A, Gabutti, G, Regoli, F, Auricchio, A. A meta-analysis of remote monitoring of heart failure patients. J. Am. Coll. Cardiol. 54, 1683–94 (2009).
7 Rivara MB, Mehrotra R. The Changing Landscape of Home Dialysis in the United States. Current Opinion in Nephrology and Hypertension.2014; 23(6):586-591.doi:10.1097/MNH0000000000000066; Mehrotra R, Chiu YW, Kalantar-Zadeh K, Bargman J, Vonesh E. Similar Outcomes with Hemodialysis and Peritoneal Dialysis in Patients with End-Stage Renal Disease. Archives of Internal Medicine. 2011; 171(2): 110-118. Doi:10.1001/archinternmed.2010.352; Ledebo I, Ronco C. The best dialysis therapy? Results from an international survey among nephrology professionals. Nephrology Dialysis Transplantation.2008;6:403-408.doi:10.1093/ndtplus/sfn148; Schiller B, Neitzer A, Doss S. Perceptions about renal replacement therapy among nephrology professionals. Nephrology News & Issues. September 2010; 36-44; Ghaffarri A, Kalantar-Zadeh K, Lee J, Maddux F, Moran J, Nissenson A. PD First: Peritoneal Dialysis as the Default Transition to Dialysis Therapy. Seminars in Dialysis. 2013; 26(6): 706-713. doi: 10.1111/sdi.12125.
8Rubin HR et al. Patient ratings of dialysis care with peritoneal dialysis vs hemodialysis. JAMA. 2004 Feb 11;291(6):697-703.
9 Juergensen, et al. Hemodialysis and peritoneal dialysis: patients’ assessment of their satisfaction with therapy and the impact of the therapy on their lives. Clin J Am Soc Nephrol. 2006; 1(6): 1191-1196.
10Zazzeroni L HR et al. Comparison of quality of life in patients undergoing hemodialysis and peritoneal dialysis: a systematic review and meta-analysis. Kidney Blood Press Res. 2017;42(4):717-727. USRDS ADR 2018: Vol 2 ESRD, Chap 5; Fig 5.1.